Understanding intercellular communication of type 2 immunity and the epithelial barrier in the lung during chronic asthma
Allergic asthma is characterized by chronic inflammation and airway remodeling, which involves epithelial barrier dysfunction, fibrosis, goblet cell hyperplasia/metaplasia, smooth muscle thickening and increased endothelial permeability.
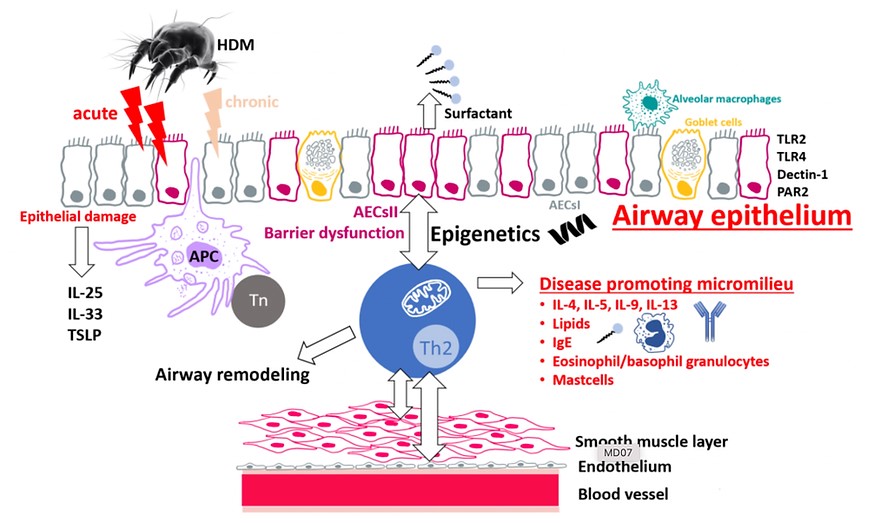
Repetitive chronic exposure to allergens such as from house dust mites (HDM) mediates a dysregulation of the airway epithelia including alveolar type II cells (AECsII). This cumulates in type 2 immune cell activation and the amplification of asthmatic airway inflammation. However, how the intercellular communication between alveolar epithelial cells and type 2 immune cells contributes to the fixation of especially chronic asthmatic airway inflammation is not fully understood yet. We hypothesize that in chronic asthma, metabolites provide a specific metabolic environment within the lung, which favors chronic inflammation and fixation of the disease by altering type 2 immunity and changing the epithelial barrier. To test this, we make use of genetically engineered mice, preclinical mouse models of asthmatic airway inflammation, single cell transcriptomics (single cell RNA sequencing), epigenetics (single cell ATAC sequencing), and metabolic analysis of alveolar epithelial cells and type 2 immune cells.






